Table of Contents
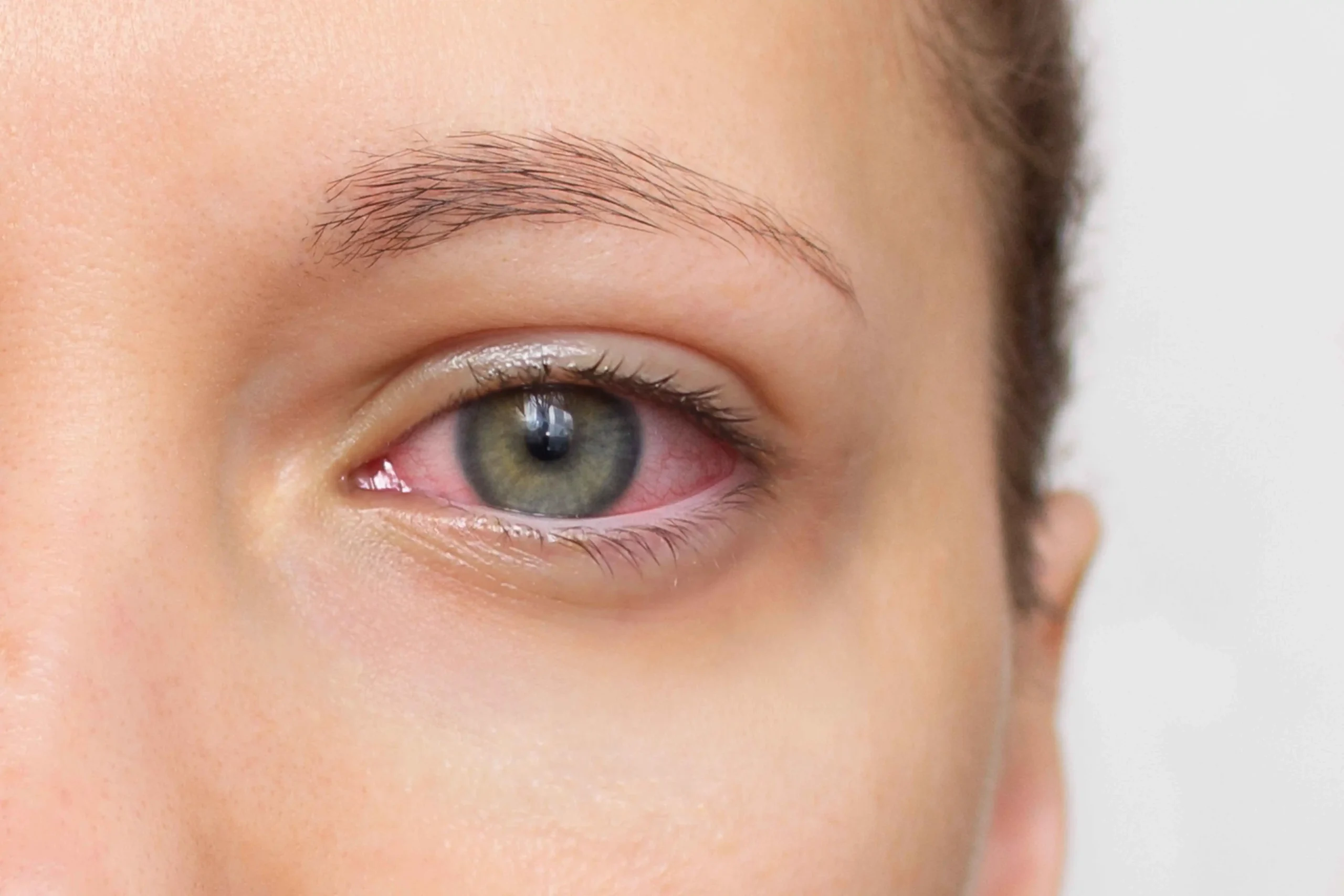
Dry Eye Disease happens when your tears lack the correct quantity, quality, or both. Healthy tears have oil, water, and mucus layers that keep the surface smooth, protect against irritants, and support clear vision. When the oil layer breaks down often from meibomian gland dysfunction tears evaporate too quickly.
The eye doesn’t have enough moisture when the water layer is low. Either way, the surface becomes inflamed and sensitive, and vision can blur, especially while reading or using digital screens. Why it matters: Untreated dryness can affect daily tasks, contact lens wear, and mood. Many people change routines around discomfort without realizing effective care exists.
Causes, Symptoms, and Treatment Options
Common causes include meibomian gland dysfunction, reduced tear production, hormonal changes, autoimmune disease, certain medications (like antihistamines and antidepressants), and environmental stressors. Skincare products and makeup can migrate to the lid margin and block glands, so technique and product choice matter.
Typical symptoms: eye inflammation and dryness, burning, stinging, gritty sensation, light sensitivity, redness, excessive tearing (yes reflex tearing can occur when the surface is dry), contact lens discomfort, and blurry vision that clears after blinking.
Treatment options span from simple to advanced:
- Daily lid hygiene and warm compresses to melt and mobilize oil.
- Preservative-free lubricants; gel or ointment at night for severe dryness.
- Prescription anti-inflammatory drops to calm the surface.
- Punctal plugs to conserve tears.
- In-clinic thermal expression to clear blocked glands.
- IPL and RF for lid margin inflammation and improved oil quality.
- Scleral lenses for severe surface disease.
- Nutritional support and lifestyle changes that reduce triggers.
Ask about dry eye therapy options that fit your routine and goals. A practical plan beats a cabinet full of unused drops. Do you want to know more? Book Norwood Park Eye Center Today! We focus on cause-based treatment, not quick fixes.
Benefits of Dry Eye Disease
The real benefits of dry eye disease come from getting a specific diagnosis and targeted treatment. You gain clarity on triggers, reduce flare-ups, and protect long-term eye surface health. People often report steadier vision throughout the day, better tolerance for screen time, and improved comfort in challenging environments, like flights or dry offices. A thoughtful plan can also cut the number of drops you rely on and reduce late-day fatigue.
Who Is This Best For?
Anyone with persistent irritation, burning, stinging, or a sandy eye feeling can benefit from an evaluation. Symptoms may worsen with extended hours on a computer, contact lens wear, makeup or skincare migrating to the lids, indoor heat or air-conditioning, and seasonal changes.
Adults over 40 experience it more often, but teens and young professionals see symptoms too, especially with heavy device use. People with autoimmune conditions, rosacea, eyelid margin disease, or a history of refractive or cataract surgery have a higher risk.
What to Expect
Pre-treatment prep
Your visit starts with a focused history: symptoms, triggers, medications, skincare, and screen habits. Testing may include tear breakup time, corneal staining, meibomian gland imaging, and inflammation markers. Small changes like switching a cleanser, adjusting contact lens wear, or adding humidity can help immediately. If you wear eye makeup, you may get tips on lid hygiene and product choices that won’t block oil glands.
Treatment day (what happens, how long, comfort level)
Your plan usually includes a mix of at-home and in-clinic options. At home, you might start with warm compresses, gentle lid cleansing, and preservative-free lubricants. In the clinic, your doctor may recommend thermal expression to clear oil glands, prescription anti-inflammatory drops, punctal plugs to retain tears, or light- and energy-based therapies.
Intense Pulsed Light (IPL) and radiofrequency (RF) can reduce eyelid margin inflammation and improve oil flow. Sessions are brief; most patients describe mild warmth and pressure rather than pain.
Downtime and recovery
Most treatments have little to no downtime. After in-clinic procedures, you can return to normal activities the same day. You may see mild redness around the lids that fades quickly. Your clinician will share simple aftercare steps, such as sun protection and gentle cleansing.
When results show, and how long they last
Some people notice relief within days to weeks, especially when inflammation settles and oil glands begin to function better. Others improve steadily over several months. Maintenance matters because triggers remain (screens, dry air, allergy seasons). That might mean brief daily care plus periodic in-clinic sessions to keep oil flow healthy and symptoms controlled.
Lifestyle Tips and Home Care
Simple habits support long-term comfort: follow the 20-20-20 rule during screen time, add a room humidifier in winter, blink fully when reading on devices, hydrate, and protect eyes from wind. Many patients appreciate natural remedies for dry eye, such as warm compresses, omega-3-rich foods, and eyelid massage use these alongside medical care for the best results.
Frequently Asked Questions
What causes Dry Eye Disease to become chronic?
Long-standing gland blockage, ongoing inflammation, and environmental stress can keep symptoms cycling. Hormonal changes and certain medications add to the mix. A stepwise plan that clears oil glands, calms the surface, and protects tears helps break the cycle and prevent future flare-ups.
What is the best dry eye disease treatment for me?
No single option fits everyone. Your doctor matches care to the root cause oil deficiency, low tear volume, or both. Plans often blend at-home hygiene, prescription drops, and in-clinic therapies like IPL or thermal expression to deliver meaningful, lasting relief.
Can I get chronic dry eye relief without relying on drops all day?
Yes. When oil glands work better and inflammation is controlled, the tear film stabilizes, and you need fewer drops. Many patients combine lifestyle changes with in-clinic care to maintain comfort through busy workdays and screen use.
Which dry eye therapy options help after screen-heavy days?
Preventive steps include the 20-20-20 rule, frequent blinking, and humidity control. Add warm compresses and periodic gland care. If symptoms persist, in-clinic treatments like IPL, RF, or thermal expression can improve oil quality and reduce flare-ups tied to device time.
Glow Up Your Eyes
Ready for clearer, more comfortable vision and a plan that fits your life? Norwood Park Eye Center offers diagnostic testing and modern therapies to calm irritation and stabilize your tears. Get Personalized Treatment for Dry Eye now and see what targeted care can do for your day-to-day comfort.